Sciatica vs Herniated Disc: What’s the Difference Between Sciatica and Herniated Disc
Lower back pain can be confusing. You feel sharp pain shooting down your leg, but you’re not sure what’s causing it.
Is it sciatica, a herniated disc, or both? Many people use these terms interchangeably, but they’re not the same thing.
Understanding the difference between sciatica and a herniated disc is crucial for getting the right treatment. Sciatica and herniated discs are two common sources of back pain, yet they represent different problems.
In this article, chiropractors with experience in sciatica and herniated disc treatment in Downers Grove break down the key theoretical and clinical differences between these conditions, including symptoms, underlying causes, and treatment approaches.
Learning to tell the difference helps you make informed decisions about your care. They’re closely connected, yet distinctly different.
This guide will help you understand the key differences between sciatica and herniated discs. We’ll explain what each one is, how they’re related, and what treatment options work best.
By the end, you’ll know exactly what’s happening in your body and how to find relief.
Understanding Sciatica: How the Sciatic Nerve Causes Back Pain

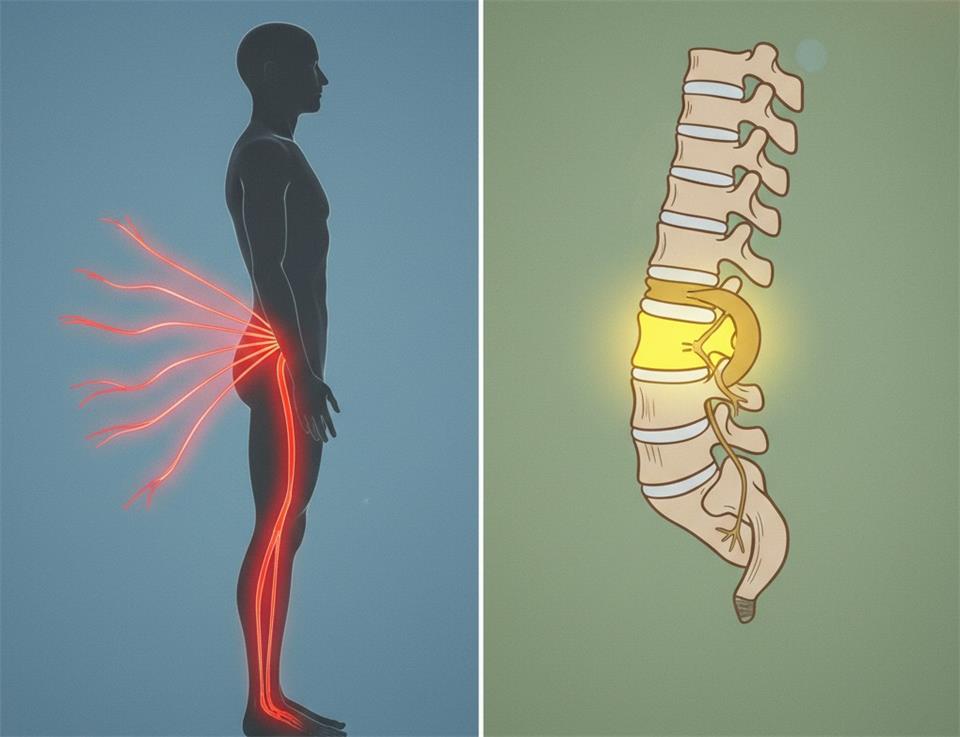
Sciatica is a set of symptoms that occur when the sciatic nerve is irritated. The sciatic nerve is the longest nerve in your body. It runs from your lower back through the hips and buttocks, then down each leg.
When this nerve becomes compressed or irritated, you experience sciatica. The pain typically affects only one side of your body.
The hallmark of sciatica is pain that shoots down your leg. It often starts in the lower back or buttock and radiates all the way to your foot. This sharp, shooting sensation is what distinguishes sciatica pain from other types of back discomfort.
Common symptoms of sciatica include numbness and tingling in the affected leg. You might also experience muscle weakness. These sensations can make walking or standing difficult.
The most common cause of sciatica is nerve compression from a herniated disc. Sciatica is often caused by a herniated disc pressing on the nerve root, which triggers the pain response. Other causes include conditions like spinal stenosis or piriformis syndrome, which create pressure on the nerve.
Sometimes muscle spasms in the lower back create enough pressure to irritate the sciatic nerve. There are also conditions with similar symptoms that can mimic sciatica, so proper diagnosis is essential.
Understanding the cause of your symptoms helps determine the right treatment approach.
What Is a Herniated Disc in Your Spine?

A herniated disc is a structural problem in your spine. Spinal discs act as cushions between the vertebrae in your spine. Each disc has a tough outer layer and contains the inner gel of a spinal disc at its center.
A herniated disc occurs when the soft inner gel pushes through a tear in the outer layer. This displaced disc material then enters the spinal canal. The spinal disc pushes against nearby nerve roots, which can cause pain.
Herniated discs most commonly occur in the lumbar spine. The lower back experiences the most movement and stress throughout the day. The cervical region in your neck is the second most common location.
Several factors can lead to disc herniation. Degenerative disc disease is a primary cause as spinal discs lose water content with age. Trauma or injury from accidents can tear the disc’s outer layer suddenly.
Repetitive strain from improper lifting or twisting also contributes to herniation. Sometimes genetics play a role in disc health and vulnerability.
Herniated disc symptoms vary widely depending on location and severity. The symptoms of a herniated disc can range from mild discomfort to severe pain. Many experience localized pain in the back at the affected area.
Numbness and muscle weakness can develop if the disc compresses a nerve. It’s possible for a herniated disc to produce no symptoms at all. Others cause severe, persistent pain that affects daily activities.
Sciatica vs Herniated Disc: Key Differences
Now let’s clarify the main distinction between these two conditions. Sciatica is a symptom caused by pressure on the nerve. A herniated disc is a structural condition in your spine.
The difference between sciatica vs herniated discs is that sciatica represents what you feel, while a herniated disc is the physical problem. Think of it this way: a herniated disc is the cause, and sciatica is the effect.
The pain pattern is the clearest way to tell them apart. Sciatica causes pain that radiates from your lower back down one leg. The sharp, shooting sensation follows the nerve pathway, sometimes reaching all the way to your foot.
Herniated disc pain, on the other hand, often stays localized in your back or neck. It may or may not radiate depending on whether the disc can cause nerve irritation.
Location also differs between the two conditions. Sciatica specifically affects your buttock, leg, and sometimes your foot. A herniated disc primarily causes problems at the spine itself, either in the lumbar or cervical region.
Here’s the critical relationship: a herniated disc can cause sciatica when it presses on the sciatic nerve root. However, it only takes a herniated disc to cause sciatica if the herniation occurs in the right location. But sciatica can also occur without any herniated disc, triggered by spinal stenosis or other conditions.
Not all herniated discs lead to sciatica. The location and severity of the herniation determine whether sciatica symptoms develop.
How Herniated Discs Compress the Sciatic Nerve and Cause Pain

When a herniation occurs in the lumbar spine, problems begin. The disc material presses against nearby nerve roots. If this pressure affects the sciatic nerve root specifically, sciatica develops.
The process involves several stages. First, the herniation creates direct compression of the sciatic nerve at the spine. This nerve compression restricts the nerve’s normal function and triggers pain signals.
Inflammation then develops around the affected nerve. Your body responds to the injury by sending inflammatory chemicals to the area. This swelling adds even more pressure on the nerve.
The irritation from both compression and inflammation sends pain signals down the leg. These signals travel along the entire length of the sciatic nerve pathway.
Location matters significantly in this relationship. A herniated disc in the lumbar region is more likely to cause sciatica. The lower spine is where the sciatic nerve roots originate.
Herniation in the upper spine causes different symptoms. It might compress other nerves but won’t trigger sciatic pain down your leg.
Diagnosis and Chiropractic Treatment Options for Sciatica and Herniated Discs

Proper diagnosis is the first step toward relief. Your doctor will start with a physical examination. They’ll test your strength, sensation, and reflexes to detect signs of nerve irritation.
Imaging tests provide a clear picture of what’s happening inside. MRI scans show detailed images of your spinal discs and nerves. CT scans can also reveal herniation and identify which nerve roots are affected.
These tests help distinguish whether sciatica or a herniated disc is the primary issue. They also rule out other conditions that produce symptoms like sciatica. An accurate diagnosis ensures you receive the right treatment plan for your specific condition.
Most cases respond well to conservative treatment options. Rest and modified activity help reduce inflammation in the early stages. You’ll want to avoid movements that worsen the pain.
Physical therapy plays a crucial role in recovery. Targeted exercises strengthen the muscles supporting your spine. Stretching improves flexibility and reduces pressure on compressed nerves.
Chiropractic care offers a non-invasive approach to sciatica treatment. Spinal adjustments can realign vertebrae and relieve pressure on pinched nerves. This hands-on treatment reduces inflammation and restores proper movement patterns.
Chiropractic treatment addresses the root cause rather than just masking symptoms. Many patients achieve effective pain relief and overcome limitations caused by sciatica through these conservative approaches.
Specialists can develop personalized treatment plans that combine multiple approaches. Your chiropractor might recommend specific exercises, lifestyle modifications, and regular adjustments. This comprehensive strategy improves your quality of life over the long term.
For persistent cases, additional treatment options exist. Epidural steroid injections can reduce severe inflammation around the nerve. These injections provide temporary relief while other treatments take effect.
Surgery is rarely needed, as most herniated discs require only conservative care. It’s typically reserved for cases where treatment hasn’t worked after several months. Procedures like microdiscectomy can remove the herniated portion of the disc pressing on the nerve.
When to Schedule an Appointment
Don’t ignore persistent back pain or leg symptoms. If your pain lasts longer than a few weeks, it’s time to seek professional help. Early intervention prevents the condition from worsening.
Certain warning signs require immediate attention. Severe numbness or muscle weakness in your leg signals serious nerve damage. Difficulty walking or standing indicates the problem needs prompt evaluation.
Loss of bowel or bladder control is a medical emergency. This symptom suggests severe nerve damage and requires immediate care.
Fill out the form to schedule an appointment with a qualified specialist. A thorough examination will determine whether sciatica or herniated discs are causing your pain. Professional diagnosis leads to the most effective treatment plan for lasting relief.



